3rd Year Voluntary Benefits: Age Lock w/New Enrollee Plans
Assumptions/Prerequisites
Minimum requirement: 1st year plans are built
• Carrier/broker has confirmed there are no changes to plan rates or eligibility criteria
• Carrier/broker has confirmed EEs will remain locked into their coverage and rates based on their original election
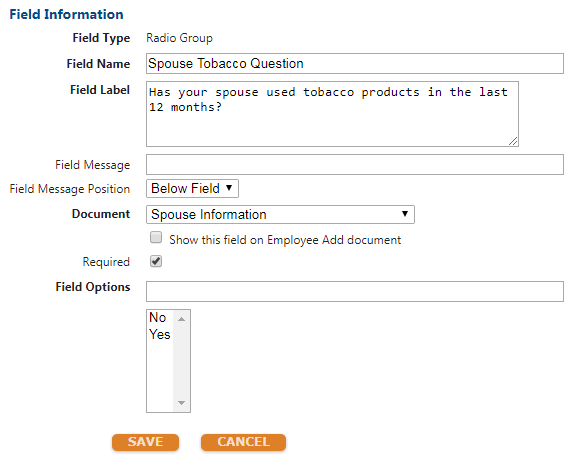
Rate Locked: EE will pay same premium year after year based on “age/years of service at plan effective date” for their original enrollment into the plan. Coverage and cost are static from original election, e.g. is as follows:
Employee Critical Illness
Offered in increments of $5,000.00
Minimum Coverage: $5,000.00
Maximum Coverage: $50,000.00
New Hire Guaranteed Issue of $15,000.00
Tobacco & Non-Tobacco Rates
Spouse Critical Illness
Offered in increments of $2,500.00
Minimum Coverage: $2,500.00
Maximum Coverage: $25,000.00 or 50% of EE coverage
New Hire Guaranteed Issue of $15,000.00
Tobacco & Non-Tobacco Rates
Child Critical Illness [Standared VB Config]
Offered in increments of $2,500.00
Minimum Coverage: $2,500.00
Maximum Coverage: $15,000.00 or 100% of EE coverage
New Hire/OE Guaranteed Issue of $7,500.00
Single rate for all dependents and equal coverage across each child
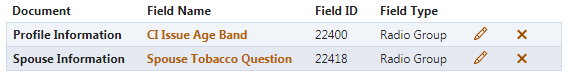
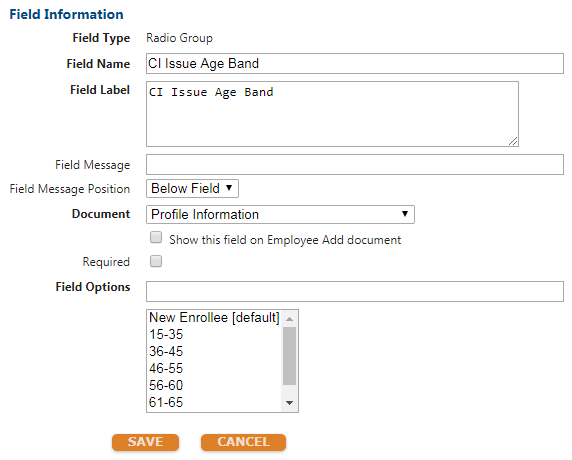
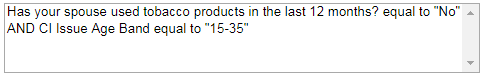
Build User Defined Fields for CI Issue Age Band & Spouse Tobacco Question to mirror the below screen shots:
Detailed Process Steps: Sample Critical Illness Site Configuration [EE/SPS]
Step 1 - Confirm Year 1 Configuration
Review the year 1 configuration after confirming prerequisites and plan configuration mentioned above.
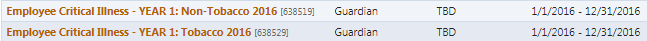
Year 1 plans should include BOTH a tobacco and non-tobacco plan, each built with a rate per $1,000.00 based on coverage.
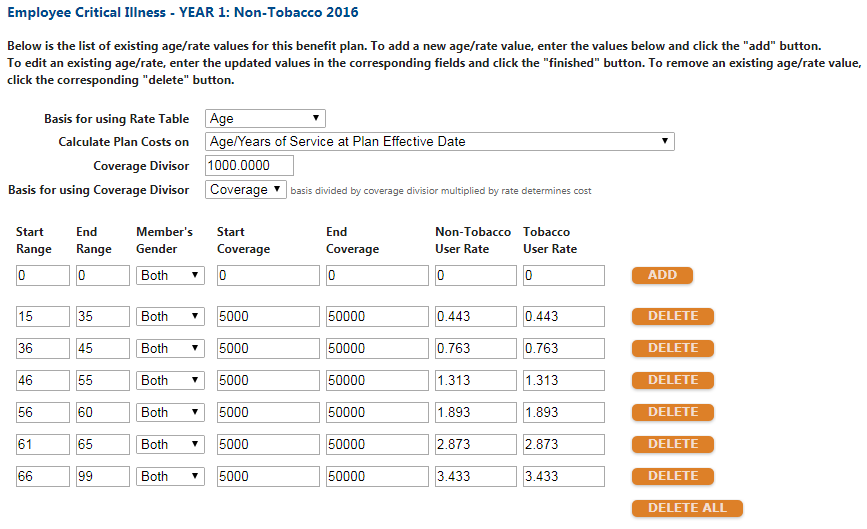
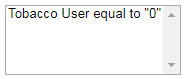
Ensure additional eligibility criteria is established for smoker/non-smoker status in the “demographic eligibility rules” section of the Eligibility Rules page.
Completed plans should appear as so:
Step 2 - Year 2 Configuration (will apply for EE and SPS plans)
Review the year 2 configuration after confirming prerequisites and plan configuration mentioned above.
Year 2 plans should include new enrollee plans for both tobacco/non-tobacco and contain a separate age band based on carrier documentation.
Each plan will carry its own rate per $1,000.00 with a range of age 0-99 to ensure rate does not change for anyone in this plan if mass update is applied OR when plans are rolled to following plan year.
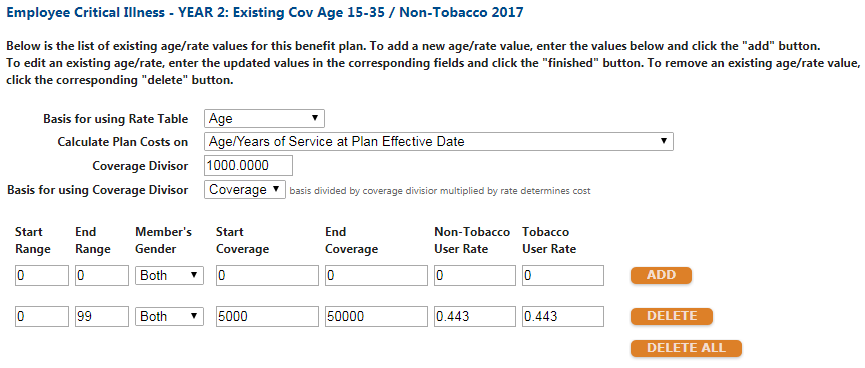
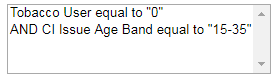
Eligibility criteria should include EE Tobacco Status AND the CI Issue Age Band that corresponds to the plan’s age band.
i. Reduction schedule should not be configured for these plans.
ii. Spouse plans will be contingent upon Spouse Tobacco UDF
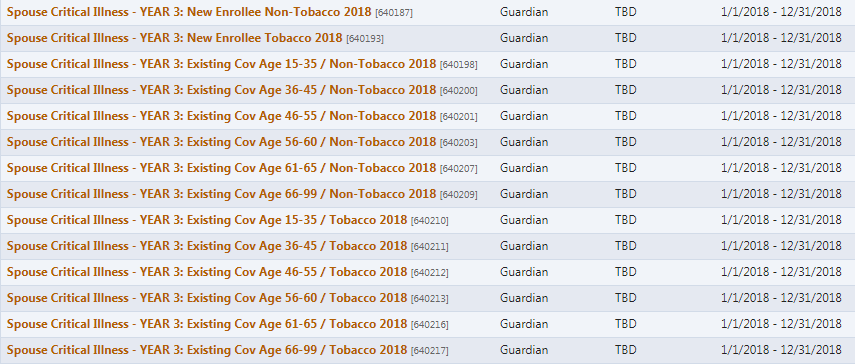
Completed year 2 plans should appear as so:


Please note: When moving to rolling elections for year 2+, CRM will need to export data from prior year’s “New Enrollee” plans and import elections into designated age band plan. This is how benefitsCONNECT will lock the rates ongoing. Each plan year when beginning open enrollment, the “New Enrollee” plans should not have any enrollment beyond test employees.
Age Reduction Consideration: Age reduction schedules should not be built out. IF a carrier has an age reduction for the plans, this will be handled via import.
Best practice will be to export a 900 from “New Enrollee” plans > manually reduce coverage and maintain rates from export > import to designated age band plan.
Step 3 - Year 3 Configuration (will apply for EE and SPS plans)
Mirror configuration for year 2 benefits.

Add plan association to prior year and future year plan designs, to roll elections to new plan year.
a. “New Enrollee” plans should not have any enrollments aside from test employee elections
b. Elections for all age bands prior to age reduction can be rolled forward to new plan year if configuration mirrors what’s been outlined above.
i. When rolling elections ensure there are no changes to rates in preview of future elections.
c. Any client that has an age reduction beginning at age 65+ will need elections exported and imported from prior year to ensure reduced coverage amounts with total coverage cost are imported and appear properly.
Updated less than a minute ago
